Dental pulpitis is a painful condition caused by inflammation of the tooth’s inner pulp, often triggered by untreated cavities or dental trauma. It can range from mild discomfort to severe, throbbing pain and may require immediate dental care if left unaddressed. Knowing the signs early and seeking treatment promptly can save your tooth and prevent complications.
Let’s explore what dental pulpitis really is, how it develops, and the best ways to manage and treat it effectively.
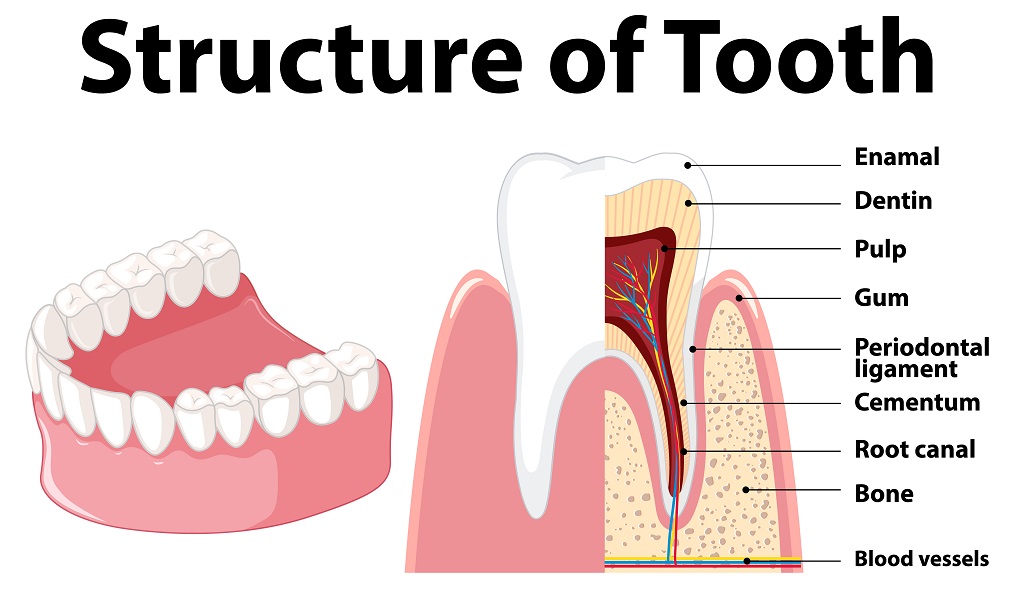
What Is Dental Pulpitis?
Dental pulpitis occurs when the pulp—the soft tissue inside your tooth that contains nerves and blood vessels—becomes inflamed. This inflammation is usually the result of bacteria entering the pulp due to deep decay, cracked teeth, or repeated dental procedures.
There are two types of dental pulpitis:
Reversible Pulpitis: The inflammation is mild and the pulp can heal on its own with proper care.
Irreversible Pulpitis: The inflammation is severe, the pulp is damaged, and the tooth will not recover without professional treatment, such as a root canal.
Common Symptoms of Dental Pulpitis
Symptoms can vary depending on the severity of the condition. Some common signs include:
Sharp, sudden pain when eating hot, cold, or sweet foods
Throbbing pain that may be spontaneous or constant
Pain that worsens when lying down or at night
Sensitivity to pressure or biting
Swelling around the affected tooth in advanced cases
In reversible pulpitis, pain typically goes away once the trigger is removed. However, in irreversible pulpitis, the pain tends to linger or intensify over time.
What Causes Dental Pulpitis?
Several factors can contribute to pulp inflammation:
Untreated Tooth Decay: Deep cavities allow bacteria to reach the pulp.
Cracked or Fractured Teeth: Openings in the enamel make it easier for bacteria to enter.
Trauma to the Tooth: A blow to the mouth can injure the pulp even if the tooth looks fine.
Repeated Dental Work: Multiple restorations on the same tooth can stress the pulp.
Gum Disease: Advanced periodontitis may lead to infection reaching the pulp tissue.
Diagnosis and Dental Evaluation
If you suspect pulpitis, your dentist will perform:
A clinical examination
X-rays to assess damage
Sensitivity tests using hot, cold, or electric stimuli
This helps determine whether the condition is reversible or irreversible, which guides treatment decisions.
Treatment Options for Dental Pulpitis
1. Reversible Pulpitis Treatment
If diagnosed early, treatment usually involves:
Removing decay and restoring the tooth with a filling
Applying desensitizing agents or fluoride to reduce sensitivity
Monitoring and maintaining good oral hygiene
With proper care, the pulp heals on its own, and pain subsides.
2. Irreversible Pulpitis Treatment
In more advanced cases, where the pulp is infected or dying, treatment includes:
Root Canal Therapy: The infected pulp is removed, and the canal is cleaned and sealed to save the tooth.
Tooth Extraction: If the damage is too extensive and the tooth cannot be restored, removal may be necessary.
Antibiotics may be prescribed if there’s significant infection or swelling, but they are not a permanent solution without further dental work.
How to Prevent Dental Pulpitis
Prevention starts with consistent oral hygiene and regular dental visits. Follow these tips:
Brush twice a day with fluoride toothpaste
Floss daily to remove plaque between teeth
Limit sugary foods and drinks
Visit your dentist every 6 months
Address cavities or dental trauma promptly
Early detection is key to preventing painful outcomes and costly procedures.
Final Thoughts
Dental pulpitis can be a warning sign that your tooth needs attention. Whether it’s a mild sensitivity or severe pain, don’t ignore the symptoms. With timely care and the right treatment, you can protect your smile and avoid further dental complications.
If you’re experiencing tooth pain that doesn’t go away, it’s time to visit your dentist—your teeth will thank you later.