Is periodontal disease curable?
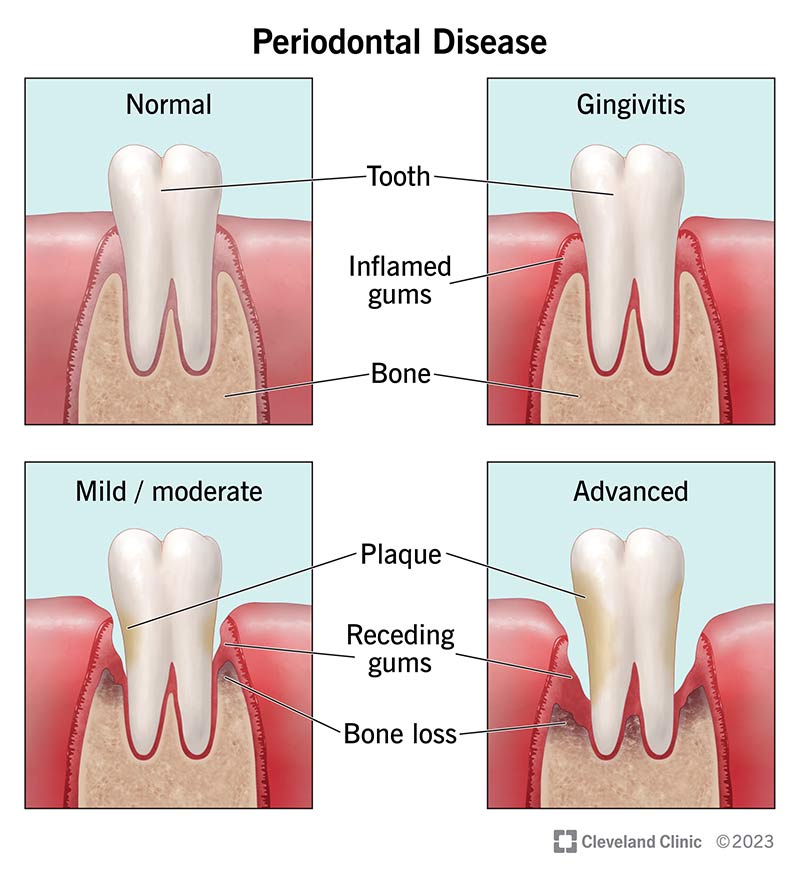
Gum disease isn’t curable, but it’s manageable with appropriate treatment. You can’t cure it because once you lose structural support around your teeth, you don’t usually get all of it back. However, periodontal treatment can reduce infection and rebuild your bone and tissue to some degree.
Another factor is genetics. There are many different types of oral bacteria. Some people are simply more prone to having the kind that causes gum disease.
One stage of gum disease is totally reversible — gingivitis (very early periodontal disease). If you detect gingivitis early enough, you can reverse it with regular dental cleaning and diligent oral hygiene.
How is periodontal disease treated?
There are several periodontal treatments available. The one that’s right for you depends on the severity of your condition and a number of other factors, including:
- Your health.
- Whether you smoke.
- What treatments you’ve had in the past.
Dental cleaning and improved oral hygiene
People who have very early periodontal disease (gingivitis) may be able to reverse the condition with routine dental cleaning and improved oral hygiene. Because there’s no bone loss yet, this conservative approach gets rid of harmful oral bacteria before the disease has a chance to progress.
Proper oral hygiene includes brushing two to three times a day, flossing daily and visiting your dentist for regular exams and cleanings.
Scaling and root planing
Scaling and root planing is similar to routine dental cleaning. But it cleans deeper beneath your gums, removing plaque and bacteria where your toothbrush and floss can’t reach. Periodontists recommend this treatment for people with mild gum disease.
During this procedure, a dental hygienist cleans (scales) the plaque from your teeth and then smooths out (planes) your root surfaces to keep bacteria from reattaching. The procedure is usually done in at least two visits using local anesthesia.
Pocket reduction surgery
People with moderate to advanced gum disease may need pocket reduction surgery (also called osseous surgery). The goal is to remove plaque and tartar that are so deep under the gums that your hygienist can’t reach it. During this procedure, a periodontist makes an incision (cut) in your gums and creates a flap. This allows them to temporarily move your gums back from your teeth roots.
Next, they’ll clean the plaque, tartar and bacteria from your teeth roots and smooth out any rough areas. Once complete, they’ll reposition your gums and close the incision with stitches.
Oftentimes, periodontists combine pocket reduction surgery with other regenerative procedures, such as bone grafting, gum grafting or guided tissue regeneration.
LANAP (Laser-assisted new attachment procedure)
Some periodontists also offer pocket reduction with LANAP. This procedure treats periodontitis using a handheld laser. The laser targets diseased gum tissue while leaving healthy tissue intact.
LANAP is a less-invasive alternative to traditional pocket reduction surgery. But results are mixed.
Bone grafting
Your periodontist may use a dental bone graft to replace bone that you’ve lost to gum disease. Once they clean the infection out, they’ll place bone grafting material into the areas where the bone has eroded. This material acts as scaffolding or a space-holder, giving your body time to regenerate its own bone over time.
Gum grafting
If you’ve lost gum tissue to periodontal disease, your dentist may recommend gum graft surgery, also called tissue grafting. This procedure covers exposed teeth roots and adds thickness to your gum line.
During this procedure, a periodontist will add tissue to the areas of gum recession. This tissue may come from the roof of your mouth, or your provider may purchase it from a licensed bone and tissue bank.
Guided tissue regeneration (GTR)
Usually, periodontists use guided tissue regeneration in combination with a bone graft. GTR helps repair periodontal defects (areas of broken-down bone) and prevents soft tissue from growing into these areas.
During GTR, a periodontist places an artificial membrane between your gums and the newly placed bone grafting material. Soft tissue regenerates faster than bone, so the membrane keeps that space open so new bone can grow there instead of soft tissue.
Platelet-rich fibrin (PRF) and platelet-rich plasma (PRP)
Platelet-rich fibrin (PRF) and platelet-rich plasma (PRP) contain growth factors that speed up healing and tissue regeneration. A periodontist can get PRF and PRP from a small sample of your blood. They’ll spin the sample in a centrifuge (a lab machine that spins rapidly, using centrifugal force) to separate plasma from your red blood cells. Then they’ll place the platelet-rich plasma or fibrin at the surgical site.
In addition to boosting healing, this type of therapy can also shorten recovery times and reduce post-surgical pain. And because it comes from your own blood, it’s completely safe.